I know what you’re thinking…
“Not again… I hated it the first time”
“But my last test was fine, do I really need to go again?”
“My friend told me that it was really painful, now I’m too scared”
“But there’s nothing wrong with me, I feel fine”
There are so many reasons why us women believe that we don’t need to go for a Pap smear. I want to separate the myths and from the facts so that you can make your own informed decision about this very important test.
But first, what is a Pap smear?
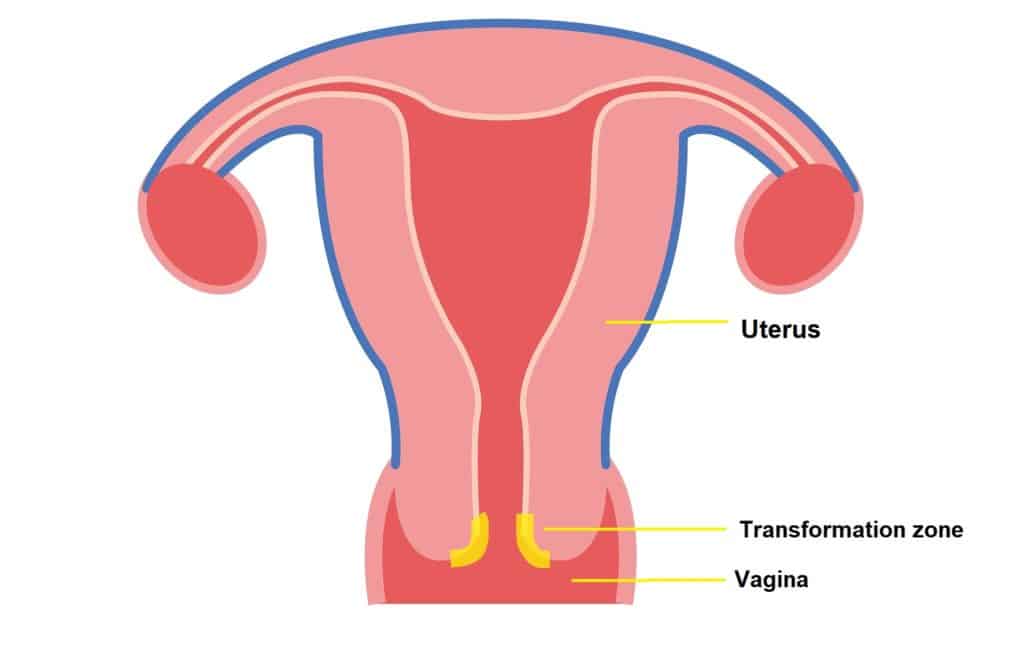
The Pap smear, or Pap test, was developed in the 1940’s by Dr George Papanicolaou. So it’s been around for quite a while. The test involves a healthcare provider lightly scraping cells from the cervix, more specifically from what is known as the transformation zone.
Oh yes, it’s anatomy time!
The transformation zone is the part of the cervix where most cervical cancers develop so we want to make sure we sample it properly. I’ve highlighted the transformation zone in the image below so you can have an idea of where it is.
Why do we keep being told to go for the test?
Well, the World Health Organisation (WHO) estimates that there were roughly 570 000 new cases of cervical cancer in 2018 alone. That’s an insane amount! They also found that the majority of deaths from cervical cancer occurred in low and middle-income countries. This can be due to having less access to healthcare and not enough pap smears being done in low income communities.
The WHO has found that Pap smears can reduce the number of deaths by cervical cancer tremendously. This is because we are able to pick up signs of cervical cancer while it’s still in the early stages, before it is actually even considered cancer yet, and cure it before it progresses. This simple test can help us stop cervical cancer right it its tracks!
How often should I get a Pap smear done?
The World Health Organisation provides us with a guideline which should be considered the minimum standard of care. This is because they need to consider the availability of healthcare resources in developing countries. More developed countries will have more resources for more frequent testing.
The WHO recommends that Pap smears be done at least once for every woman in the age group of 30-49 years.
In more developed countries, routine Pap smears begin roughly 3 years after becoming sexually active, or at the age of 21 – whichever comes first. These guidelines can vary from country to country.
For women living with HIV, the guidelines are a little different. This is because HIV can cause cervical cancer to develop earlier, progress a lot faster and may lead to an earlier death[mfn]WHO. Comprehensive Cervical Cancer Control A guide to essential practice. (2nd ed.). : World Health Organisation; 2014.[/mfn]. (Okay, things got a little morbid pretty fast…)
For women living with HIV:
- Pap smears should be done for everyone with a cervix, regardless of age, who have started engaging in sexual activity and have tested positive for HIV.
- If the results show no abnormalities, then they should repeat the test again within three years.
- For those who have been treated for precancerous cervical changes, they should come for a repeat Pap smear within the one year.
How I prepare for a Pap smear?
- Ideally you shouldn’t be menstruating when you go for your Pap smear, but if you are menstruating, don’t let it stop you from getting one if it’s your only opportunity to get tested. It can just make the test a little more difficult to interpret.
- Avoid any vaginal intercourse, douching, use of tampons, or any sort of vaginal cream (medical or otherwise) for 24-48 hours before your Pap smear.
- If you are having abnormal bleeding or discharge from the vagina before your Pap smear, don’t cancel or postpone your test because there is still a chance that those symptoms might actually be due to cervical cancer – and we definitely don’t want to miss an opportunity to catch it in time!
How does the actual procedure work?
Let me break it down for you into the different steps:
Step 1:
You will go see a healthcare provider for your Pap smear. This healthcare provider can be your local GP, a gynaecologist, a physician’s assistant or clinical associate, or a nurse trained to do Pap smears. This is important to note: You do not need to see a gynaecologist or OBGYN to do your Pap smear, unless there is another medical reason to! Save yourself the money!
Your chosen healthcare provider will ask you to lie on your back with your legs separated (this is known as the lithotomy position in the medical world) as shown below:

Image Source via ifthedevilhadmenopause
Step 2:
A lubricated speculum is inserted into the vagina to allow the healthcare provider to visualise the cervix. A speculum is a device that is used to open up and separate the walls of the vagina so that the healthcare provider can see the cervix properly before doing the test. There is one in the image below:
Image Source
This part can be slightly uncomfortable. This is usually the part that some people complain about. It’s important to remember that the vagina is a muscle, so if you tense up and squeeze your vagina closed, it will make it more difficult for the speculum to go in smoothly and quickly. This may create even more discomfort than is necessary.
As difficult as it may seem – especially with the anxiety of being exposed with your legs spread open on a table in front of a stranger – somehow you will need to relax the muscles of your vagina, also known as your Kegel muscles.
Obviously, this is much easier said than done.
This can be especially problematic if you are living with pelvic floor problems. If this is the case, I definitely recommend seeing your Sexual Medicine Specialist or OBGYN who is familiar with your specific pelvic floor condition before attempting to get a Pap smear elsewhere.
For those without pelvic floor conditions, it may be helpful to just lie back, close your eyes and focus on taking deep breaths, relaxing the muscles of your vagina. What some people find helpful is to bear down with your vagina, as if your are going to the toilet, it helps to open up the vagina and allow for easier insertion of the speculum.
In addition, make sure your healthcare provider is using enough lubricant!
Never ever underestimate the importance of lubrication when it comes to vaginas!
Unfortunately, for now there aren’t really alternative speculum options available to use for Pap smears. We are stuck with this poorly designed Cusco speculum which was designed a million years ago more for the doctor’s convenience, than for the patient’s comfort. But that is a topic for another day!
All right, Step 3:
The healthcare provider will then lightly scrape or brush the transformation zone (discussed above) with a wooden spatula or brush before transferring the cells onto a glass slide or into a liquid solution.
Step 4:
The speculum is then removed and you can get up and get dressed again. The procedure is over (and you are free!). The sample is then sent to the lab for interpretation.
It is a very short procedure, it really shouldn’t take more than five minutes.
What happens after the Pap smear?
After your Pap smear, you may experience light bleeding or spotting for the next day or two. This is because there are delicate blood vessels on the cervix which have been irritated when the sample was taken.
You also may experience some discomfort or cramps in your lower abdomen which can be similar to your usual menstrual cramps.
If you start bleeding heavily or you are experiencing severe pain, it’s important that you go see your healthcare provider urgently.
The results
How long you will wait for the results will depend on the lab and how busy they are at the time. Less busy, private laboratories may take as few as 3 days, but busy state laboratories can take up to 6 weeks.
There is a wide range of possible results, ranging from no abnormalities found to a diagnosis of cervical cancer. Fortunately, there are quite a few stages to go through before it is actually considered cancer though. We call them “pre-cancer stages” or “pre-cancerous lesions”.
When your results come back, your healthcare provider will explain your results to you and what the next step will be, depending on what was found on your Pap smear. This may involve sending you to a gynaecologist or OBGYN for further assessment.
And that’s it!
Now it’s up to you
Do you think a Pap smear is worth it? I definitely do! Let me know in the comments. Five minutes of feeling uncomfortable could actually save your life!
If you enjoyed this post or found it helpful, I’d be very grateful if you’d help by sharing it with a friend on Facebook or Twitter. Thank you!
Disclaimer: This blog contains my opinions and doesn’t reflect the opinions of the Department of Health of South Africa or The Southern African Sexual Health Association. All information is accurate and true to the best of my knowledge, but it’s possible that there may be omissions, errors or mistakes. While I am a qualified medical doctor, I am not YOUR doctor. The information presented on this blog is for entertainment and/or informational purposes only and shouldn’t be seen as professional medical advice. If you rely on any information presented, it’s at your own risk. Please consult a professional before taking any sort of action. I reserve the right to manage this blog as I see fit, including the right to remove harmful or unhelpful comments.






0 Comments
Trackbacks/Pingbacks